Joshua Strommen MD, FACEP
Many times we have heard the phrase, “life, limb, or eyesight” in reference to triaging the severity of trauma or illness that a person may have. No explanation is needed as to why our eyes are considered in the same category of importance as our arms, hands, or legs.
So how do clinicians know if your eyesight is in danger? Well, it comes down to a couple findings that can be evaluated with a physical exam and a few tools. However, most commonly, losing eyesight is of small concern to the average person with a red or painful eye because simple infections or minor trauma are the usual causes.
- Benign conditions are those where limited intervention is necessary and things like antibiotics, steroids, anti-histamines, or even watchful waiting is the treatment.
- Acutely urgent or emergent conditions may entail surgery, medicines that lower eye pressure, intra-ocular antibiotics, or even draining fluid from the eye.
- The treatment of dangerous conditions are usually under the care of an Ophthalmologist, but at times an Emergency Medicine physician may initiate eye saving treatment in the Emergency Department.
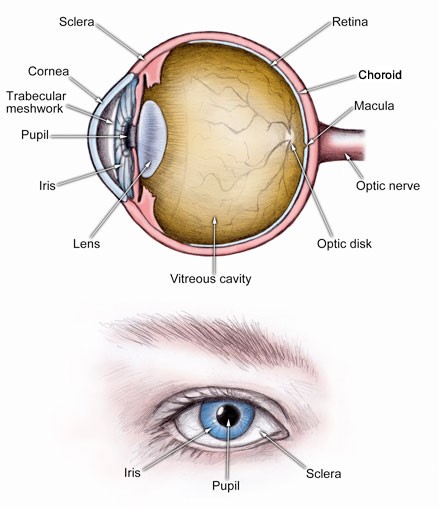
Externally, the eye is made up of the sclera, which is the white area that surrounds the iris. In the middle of the eye is the pupil, and along with the iris, a superficial layer called the cornea protects them both. Lying over the entire eye and along your eyelids is the conjunctiva. Inside the eye there are several structures that work in conjunction with nerves, arteries, and veins to give us eyesight.
What could possibly go wrong?
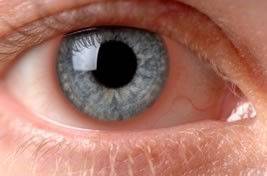
1. Conjunctivitis – This is a red, itchy, draining eye. The sclera will be red, you may have clear or mucous drainage, and you may have matting or crusting on your eyelids in the morning upon waking. Conjunctivitis can be from bacteria, viruses, or allergens.
2. Corneal abrasion – Usually occurs secondary to minor trauma to the eye, and is described as a red and painful eye that can also have tearing with it. It is diagnosed with putting a fluorescent dye in the eye under black light and seeing uptake of the dye by the cornea.
3. Keratitis – This is an infection of the cornea by either bacteria or viruses. It also presents with redness, pain, pain that’s worse with bright light, and a feeling that something is in your eye.
4. Subconjunctival hemorrhage – This is a bruise of the eye. It is a red area noted within the sclera. It occurs after being hit in the eye, or with prolonged bouts of coughing, sneezing, or vomiting.
5. Glaucoma – The 2nd leading cause of blindness in the world. This condition presents with a red, painful eye where there may be halos, headaches, and worsening of the vision.
6. Iritis – This is inflammation of the iris, and sometimes the muscles that control the lens. It is characterized by redness around the iris. There is minimal discharge and tearing. There is also photophobia or pain with bright lights in the affected AND unaffected eye.
There are a lot of overlapping symptoms within these conditions, and this is only the short list of potential eye problems. At PremiER we have all the tools to diagnose sight-threatening problems. We can also begin treatment on any of those conditions as well. We have an urgent care, which can diagnose and treat the less acute diagnoses.
It would be helpful to keep in mind these symptoms for indications of when you need to be seen by a physician:
1. Eye pain + redness
2. Photophobia – Pain with looking at light
3. Constant blurred vision
4. Eye redness + discharge













![AdobeStock_92880045 [Converted].jpg](https://images.squarespace-cdn.com/content/v1/56e0b21d8a65e25092e438a5/1485379358780-954D1C7JR6NPIIQIZ89G/AdobeStock_92880045+%5BConverted%5D.jpg)


